PROPOSD CAMPAIGN TO ‘SAVE ALL POSSIBLE LIVES & LIMBS’ IN SRI LANKA
Posted on June 9th, 2013
ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ Dr. Tilak S. Fernando ƒÆ’-¡ƒ”š‚ POW-WOW WITH DR. ATHULA WITHANAGE ƒÆ’-¡ƒ”š‚ – ƒÆ’-¡ƒ”š‚ (MD LMSSAƒÆ’-¡ƒ”š‚ Lond.,ƒÆ’-¡ƒ”š‚ FRCSƒÆ’-¡ƒ”š‚ Edin.,ƒÆ’-¡ƒ”š‚ FRCSƒÆ’-¡ƒ”š‚ Irel,ƒÆ’-¡ƒ”š‚ FRCS England FICS)
Dr. AthulaƒÆ’-¡ƒ”š‚ Withanage has been working as ƒÆ’-¡ƒ”š‚ a Consultant General & Laparoscopic Surgeon, ƒÆ’-¡ƒ”š‚ Senior Lecturer in Surgery, Hon Clinical tutor at Cardiff University Faculty, WIMAT Cardiff and retired Clinical Lead at WithybushƒÆ’-¡ƒ”š‚ GeneralƒÆ’-¡ƒ”š‚ Hospital Wales for over two decades asƒÆ’-¡ƒ”š‚ the Lead Clinician and Clinical Director who won the Clinical LeaderƒÆ’-¡ƒ”š‚ and Mentor of the year awards in 2008 and 2009 ƒÆ’-¡ƒ”š‚ from the National Health Service Trust UK . Very recently he came down to Sri Lanka on a holiday and visited ƒÆ’-¡ƒ”š‚ the ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”Green Campus, in the middle of paddy fieldsƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢, at Neville Fernando Hospital ƒÆ’-¡ƒ”š‚ at Malabe to deliver a guest lecture and commented on theƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”the most beautiful auditoriumƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ ƒÆ’-¡ƒ”š‚ as one he had never seen before anywhere in the world!
At the request of Chairmen Dr. Neville Fernando, ViceƒÆ’-¡ƒ”š‚ ChancellorƒÆ’-¡ƒ”š‚ ProfessorƒÆ’-¡ƒ”š‚ MalkanthiƒÆ’-¡ƒ”š‚ ChandrasekaraƒÆ’-¡ƒ”š‚ andƒÆ’-¡ƒ”š‚ the Dean of the medical faculty ProfessorƒÆ’-¡ƒ”š‚ ShanthiƒÆ’-¡ƒ”š‚ GunewardenaƒÆ’-¡ƒ”š‚ heƒÆ’-¡ƒ”š‚ decided to stay ƒÆ’-¡ƒ”š‚ behind in Sri Lanka to help establish the Academic Surgical unit and ƒÆ’-¡ƒ”š‚ particularly ƒÆ’-¡ƒ”š‚ to write the curriculum for the New University.
Ever since, he has helped to restructure the most modern state of the art theatre complex atƒÆ’-¡ƒ”š‚ the newƒÆ’-¡ƒ”š‚ hospital inƒÆ’-¡ƒ”š‚ Malabe.ƒÆ’-¡ƒ”š‚ He says the latest ƒÆ’-¡ƒ”š‚ look is akin to his own operating theatre in the UK, built at a cost of ƒÆ’-¡ƒ”š‚£12 million pounds from the Welsh Assembly, where he received the honour to declare open due to his involvement in designing it.
NFTH in Malabe now has theƒÆ’-¡ƒ”š‚ mostƒÆ’-¡ƒ”š‚ up toƒÆ’-¡ƒ”š‚ dateƒÆ’-¡ƒ”š‚ sophisticated electronicƒÆ’-¡ƒ”š‚ medical equipments includingƒÆ’-¡ƒ”š‚ Spiral CT as well as Colour Duplex Ultrasound Scanners with all requisite facilities to make this the best teaching hospital in the private or public sector anywhere in the country, in years to come.
DisplayingƒÆ’-¡ƒ”š‚ his ambition to work for humanity,ƒÆ’-¡ƒ”š‚ he has contributed five million rupees worth of hospital equipmentƒÆ’-¡ƒ”š‚ free of charge,ƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ the Malabe hospital which was well appreciated by the hospital directors Professor Deepal Weerasekara, Dr. Lakshan Fernando, Dr. Harsha Subashana and the Administration.ƒÆ’-¡ƒ”š‚ He says more will arrive ƒÆ’-¡ƒ”š‚ with the help of an Organisation he has formed called ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Withybush Friends of NFTHƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ ƒÆ’-¡ƒ”š‚ which will twin NFTH in Sri Lanka with WGH in UK.ƒÆ’-¡ƒ”š‚ With the popular demand of the students, he has now undertaken the task of training of budding doctors in clinical training sessions in a unique ƒÆ’-¡ƒ”š‚ and personnel style which he has developed over the years in the UK.ƒÆ’-¡ƒ”š‚ At present he uses the most up to date training video techniques until flow of patients increases to thisƒÆ’-¡ƒ”š‚ Hospital.
He took up this immense task voluntarily mainly out of concern for those well motivated youngsters, who at one stage seemed to have faced an uphill struggle.ƒÆ’-¡ƒ”š‚ He wants to be free from political involvements or arguments, but his aim being desperately to produce ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”caring and respectful doctorsƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ ƒÆ’-¡ƒ”š‚ who will place ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”patient-careƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ at the top of their list. He advises the young students at Malabe ƒÆ’-¡ƒ”š‚ that ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-the days of one minute consultation and decision making is definitely not for Malabe graduates who ƒÆ’-¡ƒ”š‚ will blossom out as ƒÆ’-¡ƒ”š‚ fully pledged doctors in the future.ƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚
HavingƒÆ’-¡ƒ”š‚ taken meƒÆ’-¡ƒ”š‚ on aƒÆ’-¡ƒ”š‚ guided tour inside theƒÆ’-¡ƒ”š‚ new hospital buildingƒÆ’-¡ƒ”š‚ byƒÆ’-¡ƒ”š‚ AthulaƒÆ’-¡ƒ”š‚ Withanage, prior to the inaugural opening,ƒÆ’-¡ƒ”š‚ I can confidently state that itƒÆ’-¡ƒ”š‚ would beƒÆ’-¡ƒ”š‚ the most up to date, modern private or government hospital in Sri Lanka.ƒÆ’-¡ƒ”š‚ The building itself is so beautiful that he called it the Tajmahal of Sri Lanka, especially when it is illuminated by flash lights in the night.
Athula Withanage is a medical manƒÆ’-¡ƒ”š‚ through andƒÆ’-¡ƒ”š‚ through toƒÆ’-¡ƒ”š‚ the inner core of his heart. With his wideƒÆ’-¡ƒ”š‚ experience inƒÆ’-¡ƒ”š‚ the medical field he is not the kind ofƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”specialistƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ƒÆ’-¡ƒ”š‚ whoƒÆ’-¡ƒ”š‚ hasƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”no timeƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ƒÆ’-¡ƒ”š‚ to listen to patients or inclined the see hundreds of patients to make his bank balanceƒÆ’-¡ƒ”š‚ growƒÆ’-¡ƒ”š‚ fat.ƒÆ’-¡ƒ”š‚ Patients who have consulted already at Malabe Hospital haveƒÆ’-¡ƒ”š‚ seen andƒÆ’-¡ƒ”š‚ feltƒÆ’-¡ƒ”š‚ the difference, the attitudeƒÆ’-¡ƒ”š‚ and theƒÆ’-¡ƒ”š‚ approach of this surgeon and his colleagues who spend moreƒÆ’-¡ƒ”š‚ timeƒÆ’-¡ƒ”š‚ with patients in discussion prior to making any medical or surgical decision.ƒÆ’-¡ƒ”š‚ He says surgery will be the last thing, after a full explanation to a patient and with his consent after the patient understanding fully what is committing to.
Athula Withanage states:ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Sri Lanka has produced the best of doctorsƒÆ’-¡ƒ”š‚ and health care workersƒÆ’-¡ƒ”š‚ in the world. Our health careƒÆ’-¡ƒ”š‚ system hasƒÆ’-¡ƒ”š‚ leaped forwardƒÆ’-¡ƒ”š‚ dramatically,ƒÆ’-¡ƒ”š‚ millions of miles, since it was established over hundred years ago. Our experts are performing the most sophisticated type of surgery and our doctors have made miracles in all fields of medicine here in Sri Lanka as well as during their work abroad.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ Sri LankanƒÆ’-¡ƒ”š‚ Government has done a lot to improve theƒÆ’-¡ƒ”š‚ servicesƒÆ’-¡ƒ”š‚ and our hospitals are getting equipped with state of the artƒÆ’-¡ƒ”š‚ equipment.ƒÆ’-¡ƒ”š‚ Yet we read about a lot of ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”near misses and loss ofƒÆ’-¡ƒ”š‚ lifeƒÆ’-¡ƒ”š‚ and limbsƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ and other horror storiesƒÆ’-¡ƒ”š‚ in the mediaƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
With all the funds allocated to National Health Services,ƒÆ’-¡ƒ”š‚ more developed countries like USA and UK,ƒÆ’-¡ƒ”š‚ tooƒÆ’-¡ƒ”š‚ haveƒÆ’-¡ƒ”š‚ experienced the same problem.ƒÆ’-¡ƒ”š‚ Only 90% of patients receive good medical care (NCEPOD REPORT 2005) with the result thatƒÆ’-¡ƒ”š‚ they haveƒÆ’-¡ƒ”š‚ opened upƒÆ’-¡ƒ”š‚ campaigns to improve the quality and safety of patient care.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-It is time we start our own campaign here in Sri LankaƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚, he firmly believes and willing to take the lead.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-The aimƒÆ’-¡ƒ”š‚ of such a schemeƒÆ’-¡ƒ”š‚ will be ƒÆ’-¡ƒ”š‚ to,ƒÆ’-¡ƒ”š‚ as much as humanly possible,ƒÆ’-¡ƒ”š‚ eradicate preventable deathsƒÆ’-¡ƒ”š‚ and life changing morbidityƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ -ƒÆ’-¡ƒ”š‚ e.g.ƒÆ’-¡ƒ”š‚ having toƒÆ’-¡ƒ”š‚ amputate a limbƒÆ’-¡ƒ”š‚ quiteƒÆ’-¡ƒ”š‚ unnecessarily; a patientƒÆ’-¡ƒ”š‚ whoƒÆ’-¡ƒ”š‚ sufferedƒÆ’-¡ƒ”š‚ a heart attack on a general wardƒÆ’-¡ƒ”š‚ dyingƒÆ’-¡ƒ”š‚ at midnightƒÆ’-¡ƒ”š‚ without basic life supportƒÆ’-¡ƒ”š‚ in the absenceƒÆ’-¡ƒ”š‚ of a professional ƒÆ’-¡ƒ”š‚ on the spotƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ and ƒÆ’-¡ƒ”š‚ withoutƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ defibrillatorƒÆ’-¡ƒ”š‚ close at hand,ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ orƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ in a ƒÆ’-¡ƒ”š‚ case ƒÆ’-¡ƒ”š‚ such as ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”a ƒÆ’-¡ƒ”š‚ young motorƒÆ’-¡ƒ”š‚ cyclist ( only child in the family) rushedƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ an emergency unitƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ inƒÆ’-¡ƒ”š‚ aƒÆ’-¡ƒ”š‚ three wheeler from Dodanduwa to KarapitiyaƒÆ’-¡ƒ”š‚ (with noƒÆ’-¡ƒ”š‚ basic first- aid facilities or supportƒÆ’-¡ƒ”š‚ inside the tutƒÆ’-¡ƒ”š‚ tutƒÆ’-¡ƒ”š‚ )ƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ whichƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ boils down toƒÆ’-¡ƒ”š‚ a single explanation -ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ beingƒÆ’-¡ƒ”š‚ too lateƒÆ’-¡ƒ”š‚ !
He emphasises :ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…- We need to get this right , we will save lives for years to come ƒÆ’-¡ƒ”š‚ and one day everyone will be grateful for introducing ƒÆ’-¡ƒ”š‚ the concept of:
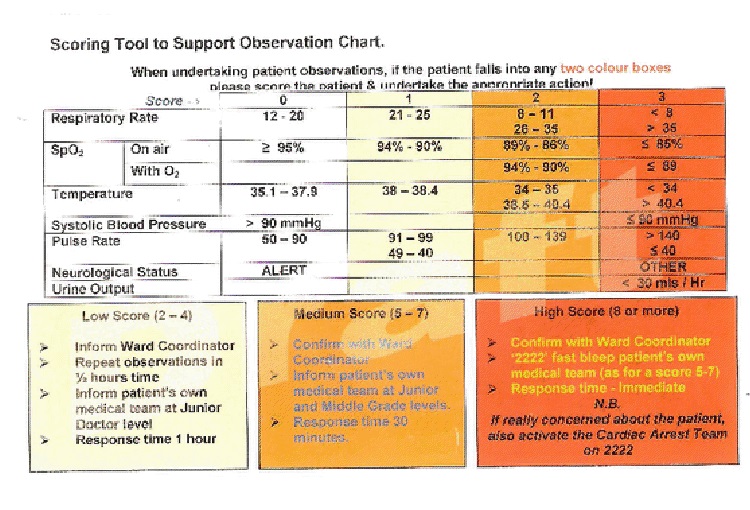
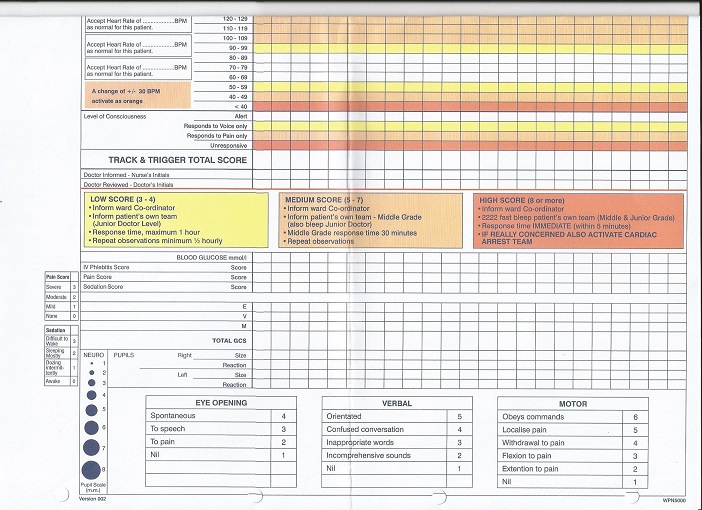
1.ƒÆ’-¡ƒ”š‚ TRAFFIC ƒÆ’-¡ƒ”š‚ LIGHT SYSTEM AND SCORE CARDS ON WARDS ( to see tiniest change to act upon preemptively)
2. ƒÆ’-¡ƒ”š‚ OUT REACH TEAM ƒÆ’-¡ƒ”š‚ to TRACK AND TRIGGER for early transfer of patients to ICU in the nick of time.ƒÆ’-¡ƒ”š‚
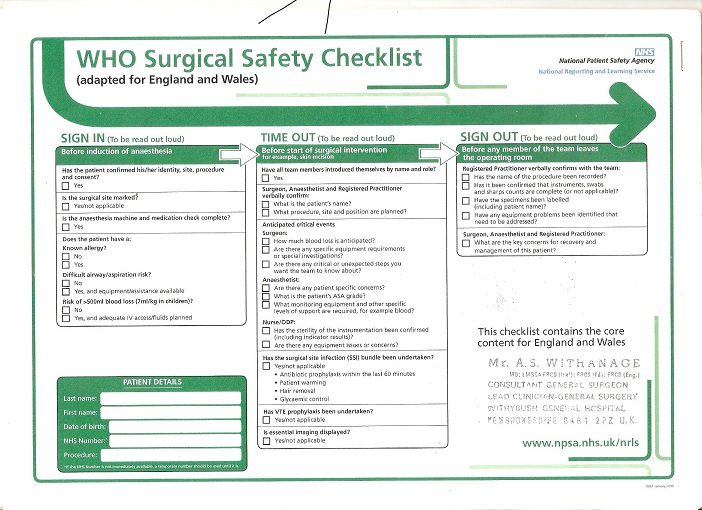
ƒÆ’-¡ƒ”š‚ 3..WHO Airline check in operation theatre
(ƒÆ’‚¢ƒ¢-¡‚¬ƒ…- For thirty years IƒÆ’-¡ƒ”š‚ haven’t lost ƒÆ’-¡ƒ”š‚ a single unexpected life or limb or ƒÆ’-¡ƒ”š‚ neverƒÆ’-¡ƒ”š‚ made an error of operating on the wrong organ as I check everything myselfƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚).
4. Effective AmbulanceƒÆ’-¡ƒ”š‚ call service in place, AT THE RIGHT site.
He was horrified recently upon hearing of a patient dying suddenly in a City Hospital in Colombo as there had not been a single staff on the ward during the night shift to resuscitate! Had that patient being in the ICU it would have been a different story, he states.
ƒÆ’-¡ƒ”š‚
CAMPAIGN TO SAVE ONE MILLION LIVES .ƒÆ’-¡ƒ”š‚
ƒÆ’-¡ƒ”š‚ USAƒÆ’-¡ƒ”š‚ hasƒÆ’-¡ƒ”š‚ startedƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”save one million lives campaignƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ƒÆ’-¡ƒ”š‚ and in EnglandƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ¢¢”š¬…”ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”save one thousand lives campaignƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢.ƒÆ’-¡ƒ”š‚ In WalesƒÆ’-¡ƒ”š‚ Athula Withanage and his team had gone beyondƒÆ’-¡ƒ”š‚ such perimetersƒÆ’-¡ƒ”š‚ and startedƒÆ’-¡ƒ”š‚ theirƒÆ’-¡ƒ”š‚ pioneering workƒÆ’-¡ƒ”š‚ onƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”save thousand lives plus campaignƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ which theyƒÆ’-¡ƒ”š‚ consideredƒÆ’-¡ƒ”š‚ asƒÆ’-¡ƒ”š‚ mother of all campaignsƒÆ’-¡ƒ”š‚ , the results of which was that his team managed to win the first price for the in the NHS Wales, UK.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ He is ever so grateful to Professor Jonathan Grey having placed complete trust on his pilot project ƒÆ’-¡ƒ”š‚ without which it would not have been possibleƒÆ’-¡ƒ”š‚ to obtain successful results.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Some have argued stating that those were ƒÆ’-¡ƒ”š‚ too ambitious targets withoutƒÆ’-¡ƒ”š‚ meaning,ƒÆ’-¡ƒ”š‚ and such campaigns were ƒÆ’-¡ƒ”š‚ already in progress, ƒÆ’-¡ƒ”š‚ and near misses could never be satisfactorily auditedƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚!
To such criticism his answer has been that ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-every medical system and its workers are proud of their work and they do their best to save millions of lives, nevertheless the inevitability of ƒÆ’-¡ƒ”š‚ one or two limbs or lives or near misses cannot be avoided out of thousands of patients who are being dealt with on a daily basis. For the individual family of course it becomes a one hundred percent disaster.ƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚
ƒÆ’-¡ƒ”š‚ Athula WithanageƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s perception is that Human life is the most precious gift human being is given and itƒÆ’-¡ƒ”š‚ needsƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ beƒÆ’-¡ƒ”š‚ protectedƒÆ’-¡ƒ”š‚ by all availableƒÆ’-¡ƒ”š‚ means. ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Dead cannot return to the clinic and complain how carelessly or badly he or she was treated orƒÆ’-¡ƒ”š‚ say how he or she missed all the truly wonderful events such as the wedding of an only daughter or celebration of a first grandchildƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s birthday! Therefore, as medical specialists what is required to achieve this target is a set of tools which is easily availableƒÆ’-¡ƒ”š‚ (notƒÆ’-¡ƒ”š‚ rocketƒÆ’-¡ƒ”š‚ science) which boils down to plain clinical parametersƒÆ’-¡ƒ”š‚ (ƒÆ’-¡ƒ”š‚ SayanikaƒÆ’-¡ƒ”š‚ MinumƒÆ’-¡ƒ”š‚ )ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-he emphasises.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-WeƒÆ’-¡ƒ”š‚ see frequently on all wards theƒÆ’-¡ƒ”š‚ observation charts, blood pressure, pulse, respiratory rate,ƒÆ’-¡ƒ”š‚ temperature,ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ oxygen saturation levels etc.,ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ whereƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ the health care workers as much as ƒÆ’-¡ƒ”š‚ patientsƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ƒÆ’-¡ƒ”š‚ relativesƒÆ’-¡ƒ”š‚ can see andƒÆ’-¡ƒ”š‚ withƒÆ’-¡ƒ”š‚ God givenƒÆ’-¡ƒ”š‚ Panchendriya.ƒÆ’-¡ƒ”š‚ If a patient complains of a pain, whichƒÆ’-¡ƒ”š‚ no doubt is aƒÆ’-¡ƒ”š‚ terrible feeling,ƒÆ’-¡ƒ”š‚ he suggests toƒÆ’-¡ƒ”š‚ give a painkiller to the patient by all means butƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ investigateƒÆ’-¡ƒ”š‚ the causeƒÆ’-¡ƒ”š‚ thoroughly and deal with the cause as a priority.ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”ƒÆ’-¡ƒ”š‚ If the wifeƒÆ’-¡ƒ”š‚ of a patientƒÆ’-¡ƒ”š‚ says ƒÆ’‚¢ƒ¢-¡‚¬ƒ…- my husband is not the same today (She knows him better than us), so ƒÆ’-¡ƒ”š‚ listen with care and investigateƒÆ’-¡ƒ”š‚ and doƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ atƒÆ’-¡ƒ”š‚ leastƒÆ’-¡ƒ”š‚ a blood chemistryƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ he suggests with ,ƒÆ’-¡ƒ”š‚ Urea and electrolytes, bloodƒÆ’-¡ƒ”š‚ sugarƒÆ’-¡ƒ”š‚ levels or any levelsƒÆ’-¡ƒ”š‚ relevantƒÆ’-¡ƒ”š‚ to patientƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s conditionƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢.ƒÆ’-¡ƒ”š‚
Clinical Parameters
ƒÆ’-¡ƒ”š‚ WhyƒÆ’-¡ƒ”š‚ areƒÆ’-¡ƒ”š‚ clinical Parameters (ƒÆ’-¡ƒ”š‚ SayanikaƒÆ’-¡ƒ”š‚ Minim) so importantƒÆ’-¡ƒ”š‚ for better outcomes in patient care?ƒÆ’-¡ƒ”š‚ In Athula WithanageƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s thinking (and every other medicƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s experience)ƒÆ’-¡ƒ”š‚ thereƒÆ’-¡ƒ”š‚ areƒÆ’-¡ƒ”š‚ always subtle and simpleƒÆ’-¡ƒ”š‚ changesƒÆ’-¡ƒ”š‚ in thoseƒÆ’-¡ƒ”š‚ clinicalƒÆ’-¡ƒ”š‚ indicators that every nurse records,ƒÆ’-¡ƒ”š‚ days or hours beforeƒÆ’-¡ƒ”š‚ the actual clinical deteriorationƒÆ’-¡ƒ”š‚ takesƒÆ’-¡ƒ”š‚ place; ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-the patient will complain if not unconscious.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ It is certainly not the early CT MRI or PET changes that are important, and that is why it is not rocket science as every nurse and every junior doctor observes this,ƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ he observes.
ICUƒÆ’-¡ƒ”š‚ Out Reach Track & Trigger Team
ƒÆ’-¡ƒ”š‚ One approach Athula Withanage started on his wardsƒÆ’-¡ƒ”š‚ during his campaign abroadƒÆ’-¡ƒ”š‚ was something calledƒÆ’-¡ƒ”š‚ theƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”ƒÆ’-¡ƒ”š‚ Traffic light systemƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ƒÆ’-¡ƒ”š‚ where normalƒÆ’-¡ƒ”š‚ levelsƒÆ’-¡ƒ”š‚ wereƒÆ’-¡ƒ”š‚ groupedƒÆ’-¡ƒ”š‚ as theƒÆ’-¡ƒ”š‚ White Zone,( anything slightly abnormal) theƒÆ’-¡ƒ”š‚ Amber ZoneƒÆ’-¡ƒ”š‚ and more abnormal indices were categorised as ƒÆ’-¡ƒ”š‚ theƒÆ’-¡ƒ”š‚ Red zone.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-ƒÆ’-¡ƒ”š‚ Within the Amber zone action and vigilance were required. ƒÆ’-¡ƒ”š‚ Healthcare workers at WGH,ƒÆ’-¡ƒ”š‚ especially nurses and junior doctors, were educated in the system at a series of general compulsory meetings at the hospitalƒÆ’-¡ƒ”š‚ with senior consultants participating and advising ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ themƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ investigate andƒÆ’-¡ƒ”š‚ inform a senior, who wasƒÆ’-¡ƒ”š‚ nextƒÆ’-¡ƒ”š‚ in line, according to the superiority ƒÆ’-¡ƒ”š‚ immediatelyƒÆ’-¡ƒ”š‚ on the slightest changeƒÆ’-¡ƒ”š‚ in patientƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s condition.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-During thisƒÆ’-¡ƒ”š‚ Pilot project two intensiveƒÆ’-¡ƒ”š‚ care nursesƒÆ’-¡ƒ”š‚ wereƒÆ’-¡ƒ”š‚ alsoƒÆ’-¡ƒ”š‚ made toƒÆ’-¡ƒ”š‚ visit generalƒÆ’-¡ƒ”š‚ wards daily toƒÆ’-¡ƒ”š‚ studyƒÆ’-¡ƒ”š‚ the observationƒÆ’-¡ƒ”š‚ chartsƒÆ’-¡ƒ”š‚ to track and trigger a patientƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s transfer to high dependency unit or even an intensive care unit before actual deterioration took place, long before multi organ failure set in.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ As they did this, a substantial team of health care workers with good intentions did not express any grievances (consultants included) which under normal circumstances would have been considered as being ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-InterfearingƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Whenever aƒÆ’-¡ƒ”š‚ patient suffered a massive heart attackƒÆ’-¡ƒ”š‚ it was common knowledge thatƒÆ’-¡ƒ”š‚ theƒÆ’-¡ƒ”š‚ life support protocols were in place and defibrillatorƒÆ’-¡ƒ”š‚ to be at close range to the patient without alarming the individual.ƒÆ’-¡ƒ”š‚ AnyƒÆ’-¡ƒ”š‚ Patient, anywhereƒÆ’-¡ƒ”š‚ onƒÆ’-¡ƒ”š‚ theƒÆ’-¡ƒ”š‚ wards,ƒÆ’-¡ƒ”š‚ was given full life support in the event of unexpectedƒÆ’-¡ƒ”š‚ cardiacƒÆ’-¡ƒ”š‚ arrest, unless a decisionƒÆ’-¡ƒ”š‚ hadƒÆ’-¡ƒ”š‚ beenƒÆ’-¡ƒ”š‚ taken not toƒÆ’-¡ƒ”š‚ do so (DNR)ƒÆ’-¡ƒ”š‚ beforehand for obvious reasonsƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.ƒÆ’-¡ƒ”š‚
Primary Care.ƒÆ’-¡ƒ”š‚
ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-AllƒÆ’-¡ƒ”š‚ familyƒÆ’-¡ƒ”š‚ doctorsƒÆ’-¡ƒ”š‚ (GPs)ƒÆ’-¡ƒ”š‚ in the NHS had toƒÆ’-¡ƒ”š‚ familiarise with ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-red flag symptomsƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ƒÆ’-¡ƒ”š‚ of all diseases e.g. cancer,ƒÆ’-¡ƒ”š‚ abnormalƒÆ’-¡ƒ”š‚ breastƒÆ’-¡ƒ”š‚ lump, bleeding from theƒÆ’-¡ƒ”š‚ rectum, and in general,ƒÆ’-¡ƒ”š‚ a specialist had to see urgent suspected cancer patients within 10 days or so in one-stop clinics and full treatment to be completed within 64 daysƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ Everyone had to go for training to learn how to break bad news sympathetically and humanely which had not been properly taught at the medical college.ƒÆ’-¡ƒ”š‚ This vital topic of care with kindness, respect empathy and learning to prioritisation will become a MUST for Malabe Medical studentsƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚, he stays quite stubbornly.
Safe Surgery Saves Life
ƒÆ’-¡ƒ”š‚ He suggestsƒÆ’-¡ƒ”š‚ that ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”all clinical parameters to be stabilised before actual ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-knifeƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ skin ƒÆ’‚¢ƒ¢-¡‚¬ƒ…- contact takes placeƒÆ’-¡ƒ”š‚ when patients go for emergency surgery or elective, ƒÆ’-¡ƒ”š‚ unless patient is notƒÆ’-¡ƒ”š‚ exsanguinatingƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ rapidly,ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ in which caseƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ the tap has to be closed.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ In his opinion, itƒÆ’-¡ƒ”š‚ is importantƒÆ’-¡ƒ”š‚ to admit such patients to ICU or anaesthetic induction areas before hand.
All elective surgical cases also must maintain normal clinical parameters, normalƒÆ’-¡ƒ”š‚ sugarƒÆ’-¡ƒ”š‚ levels, normal medicine; beta-blockers, given in the morning.
In order to prevent infections, he has always advised his team ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”to take all precautions religiously and, for same reasons, clipping of hair (Not shaving) to be done only in the anaesthetic induction roomƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢.
Other ƒÆ’-¡ƒ”š‚ areasƒÆ’-¡ƒ”š‚ highlighted at Withybush General HospitalƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ were to ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…” reduce unnecessary chatting andƒÆ’-¡ƒ”š‚ to reduce the numbers in staffƒÆ’-¡ƒ”š‚ withƒÆ’-¡ƒ”š‚ cough and coldsƒÆ’-¡ƒ”š‚ from entering theatres; everythingƒÆ’-¡ƒ”š‚ had to beƒÆ’-¡ƒ”š‚ done toƒÆ’-¡ƒ”š‚ preventƒÆ’-¡ƒ”š‚ aƒÆ’-¡ƒ”š‚ clot in legs and lungs, the so calledƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”economy class syndromeƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ where even airlinesƒÆ’-¡ƒ”š‚ today give instructions to do leg exercisesƒÆ’-¡ƒ”š‚ during flights.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ AllƒÆ’-¡ƒ”š‚ aspects of these protocols wereƒÆ’-¡ƒ”š‚ auditedƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ to find out the adherence of the staff which made Withybush to come out on top of the world leagueƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢. He was proud to say that one his Sri Lankan surgical trainees was instrumental in writing the protocol under his guidance.
Mishaps in TheatreƒÆ’-¡ƒ”š‚ -ƒÆ’-¡ƒ”š‚ WHOƒÆ’-¡ƒ”š‚ Check List (June 2008).
ƒÆ’-¡ƒ”š‚ Athula Withanage and his team took WHO check list to their heart and bravely introduced first to the Day Hospital theatre, ƒÆ’-¡ƒ”š‚ possibly first ever to do so in ƒÆ’-¡ƒ”š‚ the UK.ƒÆ’-¡ƒ”š‚ At ƒÆ’-¡ƒ”š‚ the beginning it seemed like a joke and unnecessary drama before a busy operation list, but he and his team became the pioneers in Wales in introducing theƒÆ’-¡ƒ”š‚ WHOƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Airline Take OffƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-type check list to allƒÆ’-¡ƒ”š‚ surgicalƒÆ’-¡ƒ”š‚ theatres.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-With a lot of confidence he once pronounced: ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-I am Mr. Withanage, Consultant Surgeon (Surgeons in the UK are addressed as Mr and not Dr)ƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚¦.. And I am aware of sarcasm directed towards our new concept without really understanding the idea behind. To his delight his Sri Lankan MD supervised trainees who took part in the process which proved that not only the surgeon was familiar with this all important process.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”The process, ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-sign inƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ took place before induction of anaesthesia i.e.: ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Identification of patient,ƒÆ’-¡ƒ”š‚ operationƒÆ’-¡ƒ”š‚ site ƒÆ’-¡ƒ”š‚ of patientƒÆ’-¡ƒ”š‚ and the operation identified loud and clear ƒÆ’-¡ƒ”š‚ for all to hear.ƒÆ’-¡ƒ”š‚ OperateƒÆ’-¡ƒ”š‚ on the correct side of the organ and above all, identification of the correct patient and operation had to be vitally important.ƒÆ’-¡ƒ”š‚ Expected blood loss and other concerns relevant to the individual patient were then declared. This procedure became all the more important when a distinguished eminent surgeon once removed the wrong kidney (normal kidney) of a 48 year old patient who died soon after the operation!ƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚
ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Then came the ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”Time Out – the role call and confirm Sepsis bundle and clot prophylaxis really undertakenƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Final step ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”Sign OutƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ ƒÆ’-¡ƒ”š‚ – began even before closing the wound with a SWAB count checked and operational notes and in instructions clearly recorded. All the post operative concerns were clearly documented.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-ThenƒÆ’-¡ƒ”š‚ of course,ƒÆ’-¡ƒ”š‚ back to the all important clinical parameters (Sayanika Minum) once againƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ check anyƒÆ’-¡ƒ”š‚ subtleƒÆ’-¡ƒ”š‚ changes in track and trigger until such time patient was up and about or discharged.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”Laminated cards were given to all doctors with a scoring system using clinical parameters indicating when to call the next in line according to seniority, including the consultant.ƒÆ’-¡ƒ”š‚ When there was a highest score situation the whole team was summoned.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”The knowledgeƒÆ’-¡ƒ”š‚ passed on from time to time to all concernedƒÆ’-¡ƒ”š‚ asƒÆ’-¡ƒ”š‚ how to identify sepsisƒÆ’-¡ƒ”š‚ isƒÆ’-¡ƒ”š‚ called aƒÆ’-¡ƒ”š‚ sepsis bundleƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢. Athula Withanage explained: ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-First, Golden hour sepsis care pathway duties are identified and acted upon. ƒÆ’-¡ƒ”š‚ This will clarify the diagnostic criteria, whether it isƒÆ’-¡ƒ”š‚ aƒÆ’-¡ƒ”š‚ new event like an unexpected surgical disaster – ƒÆ’-¡ƒ”š‚ e.g. bile leaksƒÆ’-¡ƒ”š‚ orƒÆ’-¡ƒ”š‚ bowel anastomosisƒÆ’-¡ƒ”š‚ leaks after gall bladder operation or due to previous infection which has flared up which involves finallyƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ investigateƒÆ’-¡ƒ”š‚ andƒÆ’-¡ƒ”š‚ find out whether any organ isƒÆ’-¡ƒ”š‚ malfunctioningƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
Key Hole Surgery
ƒÆ’-¡ƒ”š‚ Key hole surgeryƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ (laparoscopic or minimal access therapy)ƒÆ’-¡ƒ”š‚ makes a wonderful progressƒÆ’-¡ƒ”š‚ in clinical operationsƒÆ’-¡ƒ”š‚ to reduce pain. Cosmesis is beautiful without ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-cross bunƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ scars and most importantly patients get back to normal quality life and work in no time. This surgical revolution which was invented by Russians in 1910 has now become common in most leading hospitals in Sri Lanka thanks to stapling revolution (by Russians) in the 1950s and eventually by the French with video usage putting all together in the late seventies.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-One must not thinkƒÆ’-¡ƒ”š‚ thatƒÆ’-¡ƒ”š‚ clinical parameters will behave or change in a different way when there is a disaster following laparoscopic surgery.ƒÆ’-¡ƒ”š‚ SomehowƒÆ’-¡ƒ”š‚ we, the surgeons, areƒÆ’-¡ƒ”š‚ so reluctantƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ look at these patients inƒÆ’-¡ƒ”š‚ a similar way as we do in open surgeryƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ Athula Withanage states.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”Pride of a successful and comforting operation ƒÆ’-¡ƒ”š‚ must not allow us to over look at disasters happening insideƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢. TheƒÆ’-¡ƒ”š‚ magnitude and actual invasiveness of the operation is the same.ƒÆ’-¡ƒ”š‚ Only method of access is different, hence the term ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”minimal access ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”is used which needs further clarificationƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ He explains.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-In the event of a mishap all changesƒÆ’-¡ƒ”š‚ will be theƒÆ’-¡ƒ”š‚ same as before, good old clinical parameters, (SayanikaƒÆ’-¡ƒ”š‚ MinumƒÆ’-¡ƒ”š‚ )ƒÆ’-¡ƒ”š‚ temperature, pulse blood pressure, pulse oxy-meter oxygen saturations will change as before when bile leaksƒÆ’-¡ƒ”š‚ orƒÆ’-¡ƒ”š‚ bowel anastomosisƒÆ’-¡ƒ”š‚ leaks.ƒÆ’-¡ƒ”š‚ One must not wait until the ward round next day if pulse is rapid; blood pressure is low and especially if there are 800 mls of blood in the drain.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”MostƒÆ’-¡ƒ”š‚ surgeons in the UK now refer to the inordinate delays in the arrival of CT scan confirmation reports and actions as theƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-doughnutƒÆ’-¡ƒ”š‚ of deathƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.ƒÆ’-¡ƒ”š‚ AthulaƒÆ’-¡ƒ”š‚ Withanage states that, ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-ƒÆ’-¡ƒ”š‚ there is no harm to act immediately with the gut feeling , but a wise surgeon willƒÆ’-¡ƒ”š‚ look in with laparoscope, ƒÆ’-¡ƒ”š‚ wash and put a drain or open before every organƒÆ’-¡ƒ”š‚ in the bodyƒÆ’-¡ƒ”š‚ ceases to function, ƒÆ’-¡ƒ”š‚ although the ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…” big surgeon big incisionƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ days are over. When the clinical picture tells you to open, you open and close the tap if bleeding or plug the hole if leakingƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
In Wales he had introduced a ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”Disaster DayƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ where surgeons from all over Wales met on a particular day to discuss any disasters and experiences openly ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ honouring patient confidentiality. ƒÆ’-¡ƒ”š‚ It was a kind of Mortality and Morbidity meeting to learn from their mistakes.ƒÆ’-¡ƒ”š‚ Equally they were not ashamedƒÆ’-¡ƒ”š‚ of to discussƒÆ’-¡ƒ”š‚ everythingƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ on this particular day in analysing chronologicallyƒÆ’-¡ƒ”š‚ to find outƒÆ’-¡ƒ”š‚ whatever had led toƒÆ’-¡ƒ”š‚ any patientƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢sƒÆ’-¡ƒ”š‚ death (No names were disclosed except patientsƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ initials and age). ƒÆ’-¡ƒ”š‚ DVD recordings of the operation were rolled back to identify what exactly had gone wrong in the case of any detailed information required. On the DisasterƒÆ’-¡ƒ”š‚ DayƒÆ’-¡ƒ”š‚ surgeons from all parts ofƒÆ’-¡ƒ”š‚ WalesƒÆ’-¡ƒ”š‚ presented their cases as teamsƒÆ’-¡ƒ”š‚ to emphasise and how to avoid any adversity in the future.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-All hospital work asƒÆ’-¡ƒ”š‚ well as any taskƒÆ’-¡ƒ”š‚ anywhere else in the community is team work.ƒÆ’-¡ƒ”š‚ If we are all good team players we can do an excellent job;ƒÆ’-¡ƒ”š‚ to blame one person alone isƒÆ’-¡ƒ”š‚ akinƒÆ’-¡ƒ”š‚ to washing oneƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s hand of oneƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s responsibilities,ƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ he believes.
Ambulance services.ƒÆ’-¡ƒ”š‚
ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”These are the days of super highways and supersonic air aircraft; therefore, it is vital to bring all seriously ill patientsƒÆ’-¡ƒ”š‚ in a ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”well stabilisedƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ƒÆ’-¡ƒ”š‚ condition at rocket speedƒÆ’-¡ƒ”š‚ to all district hospitals.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ Sri Lanka recentlyƒÆ’-¡ƒ”š‚ acquired 250 ambulances, adding to existing stock at various hospitals in the country.ƒÆ’-¡ƒ”š‚ But the amazing factor is thatƒÆ’-¡ƒ”š‚ in most cases of emergencies or accidents on the roadƒÆ’-¡ƒ”š‚ three wheelers, devoid of any life support, primary care or stabilising any clinical parameters, are still being used to takeƒÆ’-¡ƒ”š‚ criticallyƒÆ’-¡ƒ”š‚ illƒÆ’-¡ƒ”š‚ with multiplyƒÆ’-¡ƒ”š‚ injured patients to hospitals.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ This was clearly demonstrated in the news media a few days ago where a pregnant mother who was being taken to a hospital in her labour, over ƒÆ’-¡ƒ”š‚ a considerable distance, ƒÆ’-¡ƒ”š‚ by a three wheeler ƒÆ’-¡ƒ”š‚ and dying without any life supportƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Another drawback in Sri Lanka is the absence of a general emergency number allocated solely ƒÆ’-¡ƒ”š‚ to heath care functions such as ƒÆ’-¡ƒ”š‚ calling an ambulance in an emergency situation (barring private ambulance services which are also parked in hospital premises). All TV channels must give this information free of charge from time to time,ƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ he stresses.
Health Department ambulancesƒÆ’-¡ƒ”š‚ areƒÆ’-¡ƒ”š‚ parked at main district hospitalsƒÆ’-¡ƒ”š‚ only toƒÆ’-¡ƒ”š‚ transfer patients from hospital to hospital and not from the place of injury or from a site where a sudden and severe illness was reported.ƒÆ’-¡ƒ”š‚ In this scenario Athula Withanage poses the question: ƒÆ’‚¢ƒ¢-¡‚¬ƒ…- Are ƒÆ’-¡ƒ”š‚ weƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ going to allow to continually ƒÆ’-¡ƒ”š‚ loseƒÆ’-¡ƒ”š‚ any lives (especially ƒÆ’-¡ƒ”š‚ the seriously injured accident victimsƒÆ’-¡ƒ”š‚ due to renal shut down due to delay or ƒÆ’-¡ƒ”š‚ exanguinationƒÆ’-¡ƒ”š‚ as a result of unavailability of primaryƒÆ’-¡ƒ”š‚ onsiteƒÆ’-¡ƒ”š‚ treatment and being unable to stabilise and transfer patients with continuing life support toƒÆ’-¡ƒ”š‚ a hospital in timeƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢.
AthulaƒÆ’-¡ƒ”š‚ WithnageƒÆ’-¡ƒ”š‚ throws out many other questions which are food for thought:ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Are we going to miss out on the ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Golden hourƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ whereƒÆ’-¡ƒ”š‚ we could do more to save life?ƒÆ’-¡ƒ”š‚ Obstruction to airway kills before lack of breathing and there is no breathing before circulation,ƒÆ’-¡ƒ”š‚ yetƒÆ’-¡ƒ”š‚ occasionallyƒÆ’-¡ƒ”š‚ may need to close the tap of haemorrhage to save a life on the spot.ƒÆ’-¡ƒ”š‚
ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-This is theƒÆ’-¡ƒ”š‚ ABC that every medical studentƒÆ’-¡ƒ”š‚ should know, but when are we going to really practice this action?ƒÆ’-¡ƒ”š‚ HowƒÆ’-¡ƒ”š‚ manyƒÆ’-¡ƒ”š‚ trainedƒÆ’-¡ƒ”š‚ first-aidƒÆ’-¡ƒ”š‚ workers areƒÆ’-¡ƒ”š‚ aroundƒÆ’-¡ƒ”š‚ usƒÆ’-¡ƒ”š‚ inƒÆ’-¡ƒ”š‚ everyƒÆ’-¡ƒ”š‚ office, everyƒÆ’-¡ƒ”š‚ factory, every school every playground, every police station,ƒÆ’-¡ƒ”š‚ and inƒÆ’-¡ƒ”š‚ every area and in hospitals?ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ Are our junior doctors getting trained for basic life support every five years orƒÆ’-¡ƒ”š‚ so?ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ For that matter we,ƒÆ’-¡ƒ”š‚ asƒÆ’-¡ƒ”š‚ consultants tooƒÆ’-¡ƒ”š‚ shouldƒÆ’-¡ƒ”š‚ undergoƒÆ’-¡ƒ”š‚ some training from timeƒÆ’-¡ƒ”š‚ to time.ƒÆ’-¡ƒ”š‚ In most countries all surgical seniors go through a valid advance life support certificate, (at least some training. ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ TheseƒÆ’-¡ƒ”š‚ daysƒÆ’-¡ƒ”š‚ defibrillators in the advisory mood talk to us,ƒÆ’-¡ƒ”š‚ rest is hands-on training skills in labs ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-.
He poses a vital question: ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Are ambulances kept in the right place to start with? ƒÆ’-¡ƒ”š‚ Are we actually using ambulancesƒÆ’-¡ƒ”š‚ for hospital to hospital patient transfer only?ƒÆ’-¡ƒ”š‚ ShouldnƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢tƒÆ’-¡ƒ”š‚ the ambulancesƒÆ’-¡ƒ”š‚ be kept in other smallerƒÆ’-¡ƒ”š‚ hospitalsƒÆ’-¡ƒ”š‚ or evenƒÆ’-¡ƒ”š‚ atƒÆ’-¡ƒ”š‚ police stationsƒÆ’-¡ƒ”š‚ as patients need toƒÆ’-¡ƒ”š‚ beƒÆ’-¡ƒ”š‚ transferred fromƒÆ’-¡ƒ”š‚ any areaƒÆ’-¡ƒ”š‚ toƒÆ’-¡ƒ”š‚ the nearest hospital?ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ Our security forces are well trained in most life support procedures andƒÆ’-¡ƒ”š‚ policeƒÆ’-¡ƒ”š‚ tooƒÆ’-¡ƒ”š‚ have some trainingƒÆ’-¡ƒ”š‚ to a certain degree.ƒÆ’-¡ƒ”š‚ AsƒÆ’-¡ƒ”š‚ PoliceƒÆ’-¡ƒ”š‚ are the first to arriveƒÆ’-¡ƒ”š‚ on a critical scene,ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ is there any harmƒÆ’-¡ƒ”š‚ in giving some regular training to a few police officers,ƒÆ’-¡ƒ”š‚ in addition to theirƒÆ’-¡ƒ”š‚ normalƒÆ’-¡ƒ”š‚ duties andƒÆ’-¡ƒ”š‚ retain anƒÆ’-¡ƒ”š‚ ambulanceƒÆ’-¡ƒ”š‚ in every police station?ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ This willƒÆ’-¡ƒ”š‚ alsoƒÆ’-¡ƒ”š‚ cutƒÆ’-¡ƒ”š‚ down on additional expenditure andƒÆ’-¡ƒ”š‚ save moneyƒÆ’-¡ƒ”š‚ to maintain ambulance crews as well. In this manner, police will not only control the crowds in such an event but also save livesƒÆ’-¡ƒ”š‚ as they are ƒÆ’-¡ƒ”š‚ the one always arrive first on the sceneƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”Life styleƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ƒÆ’-¡ƒ”š‚ Clinics.
ƒÆ’-¡ƒ”š‚ ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-In Sri Lanka doctors are doing wonderfulƒÆ’-¡ƒ”š‚ miraclesƒÆ’-¡ƒ”š‚ to save lives.ƒÆ’-¡ƒ”š‚ So many campaigns have begun especiallyƒÆ’-¡ƒ”š‚ onƒÆ’-¡ƒ”š‚ diabetic control, kidney diseases, worldƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s best malaria eradication campaign etc.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ The Government has done an immense task in buildingƒÆ’-¡ƒ”š‚ state of the art hospitalsƒÆ’-¡ƒ”š‚ and isƒÆ’-¡ƒ”š‚ opening moreƒÆ’-¡ƒ”š‚ and more. Colombo General Hospital recently opened another new ƒÆ’-¡ƒ”š‚ wing. ƒÆ’-¡ƒ”š‚ Similarly the general public also need toƒÆ’-¡ƒ”š‚ contributeƒÆ’-¡ƒ”š‚ more to change their life styleƒÆ’-¡ƒ”š‚ and help to cut down on additional expenses on the health budget by refraining from smoking and maintaining good health byƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ walkingƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ regularlyƒÆ’-¡ƒ”š‚ andƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ eatingƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ a healthy dietƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-ƒÆ’-¡ƒ”š‚ If someone hasƒÆ’-¡ƒ”š‚ crampƒÆ’-¡ƒ”š‚ in his leg due to narrowing or furring of an artery, theƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ likelihoodƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ ofƒÆ’-¡ƒ”š‚ him loosing that legƒÆ’-¡ƒ”š‚ in a year is approx. 1%ƒÆ’-¡ƒ”š‚ -ƒÆ’-¡ƒ”š‚ 2%, but you can almost predict at least 59% will be dead in five years time following a heart attack or a stroke.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ This fact one must understand clearly, ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ Change in life style must take today not when one has pain in the chest ƒÆ’-¡ƒ”š‚ when running ƒÆ’-¡ƒ”š‚ to the bus or fallen in the bath behind closed doors and ƒÆ’-¡ƒ”š‚ paralysed with a massive strokeƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-ƒÆ’‚¢ƒ¢-¡‚¬ƒ”¹…”Life styleƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ƒÆ’-¡ƒ”š‚ clinicsƒÆ’-¡ƒ”š‚ areƒÆ’-¡ƒ”š‚ not only for diabetic centresƒÆ’-¡ƒ”š‚ but must spring upƒÆ’-¡ƒ”š‚ in all parts ofƒÆ’-¡ƒ”š‚ theƒÆ’-¡ƒ”š‚ country.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ A nurse,ƒÆ’-¡ƒ”š‚ dietician, psychologistƒÆ’-¡ƒ”š‚ andƒÆ’-¡ƒ”š‚ aƒÆ’-¡ƒ”š‚ doctor,ƒÆ’-¡ƒ”š‚ to do the clinical and vascular examination and a few fasting blood tests, areƒÆ’-¡ƒ”š‚ all thatƒÆ’-¡ƒ”š‚ isƒÆ’-¡ƒ”š‚ required. Blood pressure manometer, hand held DopplerƒÆ’-¡ƒ”š‚ areƒÆ’-¡ƒ”š‚ theƒÆ’-¡ƒ”š‚ minimal equipment that isƒÆ’-¡ƒ”š‚ required.ƒÆ’-¡ƒ”š‚ As a team, these four can visit various offices, factoriesƒÆ’-¡ƒ”š‚ or set up such clinics at a minimal cost to the targeted groups at variousƒÆ’-¡ƒ”š‚ venuesƒÆ’-¡ƒ”š‚ around the country to nip something serious in the bud and save enormous amount of money for our health service.ƒÆ’-¡ƒ”š‚ Nations health is also definitely reflects in the productivity of the country.
Various expensive scans – e.g. CT, or MRI scans are not always required.ƒÆ’-¡ƒ”š‚ Doing just CT to give one a clean bill of health is just a misguided notion although good for business in the private sectorƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚ he emphasises.
Blame Game
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Blame game has never workedƒÆ’-¡ƒ”š‚ anywhere in the world.ƒÆ’-¡ƒ”š‚ What we need to do is look carefully at various resources and to find out whether there is a critical mass of health care workers at each location?ƒÆ’-¡ƒ”š‚ Are there enough equipmentƒÆ’-¡ƒ”š‚ andƒÆ’-¡ƒ”š‚ drugs available at every site?ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚ Are we giving enough rest, enough hands-on training to staff and retraining all our health careƒÆ’-¡ƒ”š‚ workers from time to time?ƒÆ’-¡ƒ”š‚ Are we rewardingƒÆ’-¡ƒ”š‚ special life savers and do we recognise people with leadership qualities and unsung heroes in our systemƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚?
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…- Every attempt must be taken not to disfigure a patientƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢s faculty ƒÆ’-¡ƒ”š‚ like ƒÆ’-¡ƒ”š‚ in the case of the young university student who lost her limb recently ƒÆ’-¡ƒ”š‚ or must not allow ƒÆ’-¡ƒ”š‚ the only child in a family ƒÆ’-¡ƒ”š‚ to lose his/her life ƒÆ’-¡ƒ”š‚ because we cannot take them to a hospital in time.ƒÆ’-¡ƒ”š‚ Discipline must be implemented everywhere – in the schools, universities, markets, assembly halls and most importantly ƒÆ’-¡ƒ”š‚ on the roads where bus drivers need to take a greater responsibility on passengersƒÆ’‚¢ƒ¢-¡‚¬ƒ¢-¾‚¢ lives they transport as well as the pedestrians on the road.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…- Primary prevention and secondary prevention of accidents waiting to happen must be looked in to by all citizens. This is the duty of every citizen and not only of the doctors!ƒÆ’-¡ƒ”š‚ We must not let a four year old fall into a bath tub or unprotected well and die.ƒÆ’-¡ƒ”š‚ All Samaritans must proactively save lives of our citizens regardless of their religion nationality or race.ƒÆ’-¡ƒ”š‚ Sri Lanka is a country with no frequent natural disasters, so let us live happily without any unnecessary and avoidable trauma till the end of our daysƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Now thatƒÆ’-¡ƒ”š‚ theƒÆ’-¡ƒ”š‚ unimaginable and cruel suffering of the war is over for all of us, let today be the day of peace and tranquillity and then for ever. Our religious leaders from all faithsƒÆ’-¡ƒ”š‚ haveƒÆ’-¡ƒ”š‚ to play aƒÆ’-¡ƒ”š‚ responsibleƒÆ’-¡ƒ”š‚ role starting from the very young to the knownƒÆ’-¡ƒ”š‚ grown-upƒÆ’-¡ƒ”š‚ wrong doers.
ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Enough is enough;ƒÆ’-¡ƒ”š‚ thisƒÆ’-¡ƒ”š‚ is aƒÆ’-¡ƒ”š‚ great countryƒÆ’-¡ƒ”š‚ andƒÆ’-¡ƒ”š‚ certainly not a killing field. So let ƒÆ’‚¢ƒ¢-¡‚¬ƒ…-Let us start theƒÆ’-¡ƒ”š‚ SAVE ALL POSSIBLE LIVES AND LIMBS CAMPAIGN IN SRI LANKAƒÆ’-¡ƒ”š‚ earnestly todayƒÆ’‚¢ƒ¢-¡‚¬ƒ”š‚.ƒÆ’-¡ƒ”š‚ ƒÆ’-¡ƒ”š‚
ƒÆ’-¡ƒ”š‚ tilakfernand@gmail.com

June 9th, 2013 at 10:53 pm
please send this to all Australian hospitals, which are grossly mismanaged, especially emergency. doctors basically are poor managers, and the worst in the world are aussie doctors and specialists.
June 11th, 2013 at 8:54 pm
Very well written useful information Dr Athula, This is important not only for budding doctors like me, but also to all the political state governors to start thinking…!